What is Uveitis?
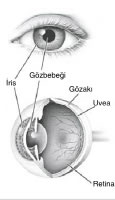
The gel-like substance located in the center of the eyeball is surrounded by a three-layered sheath. The middle layer is called the "Uvea." Inflammation of the uvea is called "Uveitis." Uveitis can affect all or any part of the eye’s layers, namely the iris, choroid, and ciliary body, which are collectively referred to as the uvea.
The uvea is now considered a separate field of specialization in eye care. The diagnosis and treatment of uvea-related diseases are supported by the growing advancements in immunology and genetics.
The key factors contributing to successful treatment include early diagnosis, regular follow-ups, a good patient-doctor relationship, and appropriate treatment. When these conditions are met, the eye can often be saved.
Even after treatment is completed, the patient should be monitored at least once every three months. Since the disease can silently recur, regular check-ups are essential. It is also necessary to inform the eye doctor about other symptoms related to different organs. For example, mouth ulcers, skin spots, or rheumatic symptoms.
Uveitis is a highly complex disease and can follow a different course in each patient. The treatment, like the course of the disease, is personalized. The dosage of medication to be used should be determined by an ophthalmologist who is specialized and experienced in uvea conditions.
Causes of Uveitis: In 30-40% of uveitis cases, the exact cause cannot be identified. Uveitis can be caused by agents such as viruses, fungi, and parasites, or it can be a symptom of a systemic disease in the body that manifests in the eyes. Therefore, various tests are required to investigate underlying conditions. Uveitis can also develop alongside systemic diseases related to collagen tissue or autoimmune disorders. Examples include Behçet's disease, ankylosing spondylitis, and rheumatoid arthritis.
 Conditions that Can Lead to Uveitis:
Conditions that Can Lead to Uveitis:
- Behçet's Disease
- Infections (bacteria, viruses, parasites, or fungi) can spread from other areas to the eye, such as tuberculosis, syphilis, herpes, toxoplasmosis, etc.
- Eye Trauma and Surgeries
- Autoimmune reactions (immune system disorders), rheumatic diseases, ulcerative colitis, sarcoidosis.
Symptoms of Uveitis:
When uveitis occurs in the front part of the eye, during severe episodes, it presents with symptoms such as redness, blurred vision, pain around the eye, light sensitivity, and floaters. When uveitis affects the back part of the eye, symptoms are mostly limited to blurred vision. If uveitis involves the central vision area, sudden vision loss and permanent vision impairment due to tissue damage can occur. Damage in uveitis outside the central area does not cause permanent vision loss unless the macula is affected.
- Vascularization and edema in the iris
- Constriction of the pupil
- Inflammatory cells behind the lens and in front of the vitreous
- Increasing headaches
- Decreased or blurred vision
- Severe eye pain
- Light sensitivity and glare
- Redness in the eye
- Tearing
- Spots in the visual field
- Sudden light flashes
Types of Uveitis:
How is Uveitis Diagnosed?
Uveitis is an urgent medical condition regardless of severity. If not addressed promptly, the disease progresses and can cause permanent effects such as pupil shape distortions, cataracts, and increased intraocular pressure due to inflammation. Once symptoms begin, the first step is to see an ophthalmologist experienced in uveitis. Delaying the initial examination can lead to permanent vision loss.
Some types of uveitis have typical appearances, making immediate diagnosis possible. However, if the back portion of the eye is involved, advanced techniques like angiography, ultrasonography, and electroretinography (ERG) may be necessary to understand the severity of the threat to vision and monitor treatment efficacy. For instance, angiographies with ICG (indocyanine green) dye can provide direct diagnostic information in suspicious cases.
Further investigations may be done in collaboration with specialists such as rheumatologists, pulmonologists, dermatologists, and neurologists.
Behçet’s Disease
Behçet's disease, first described in 1937 by Turkish dermatologist Prof. Dr. Hulusi Behçet, is a chronic condition that causes ulcers in the mouth and genital regions and inflammation (uveitis) in the eyes. It most commonly affects people living in regions known as the Silk Road, including Mediterranean countries, Israel, Japan, and recently, Turkey.
In addition to these major symptoms, Behçet’s disease can have destructive effects on other organs such as large vessels, the central nervous system (brain), joints, skin, digestive system, lungs, etc.
Given the severity of Behçet's disease, even if only one or two symptoms appear initially, the patient is monitored and treated for "suspected Behçet's disease." It is not necessary for all symptoms to be present at the same time.